Risk Assessment & Programming (RAP) Toolkit
Introduction
The Risk Assessment and Programming (RAP) Toolkit is a simple, lightweight resource that supports the creation of EMS-driven public health initiatives.
EMS agencies and public health organizations address community health needs in distinct, different ways. Public health organizations work proactively and broadly across populations to try and prevent injuries or illnesses before they happen. In contrast, EMS agencies work reactively and treat injuries and disease in a one-on-one approach during 9-1-1 requests from their community.
Despite these different approaches, both groups often find themselves addressing similar community health issues — infectious diseases, child injuries, senior injuries, substance use, and so much more. It is in these areas of shared focus, where EMS and public health collaborations make a great deal of sense.
This is the core purpose of the RAP Toolkit — to highlight areas of shared interest and promote collaboration that will accelerate both EMS and public health efforts. The RAP Toolkit is comprised of multiple RAP Tools, with each RAP Tool focusing on a different community health issue.
We have built this tutorial to show you the functional anatomy of RAP Tools and how they qualify, quantify, and suggest programming for each of these community health issues. Additionally, we have included primer information on the history of EMS prevention and different types of EMS public health initiatives. These topics will help you understand where the RAP Toolkit came from and how it works.
We hope these resources aid you in your efforts to establish proactive EMS initiatives!
A (Very) Brief History of EMS Prevention
The idea of EMS and public health partnership was first brought to national attention in the mid-1990s. At the time, EMS was a relative newcomer to the healthcare space. It had only been a little more than two decades since EMS's inception. EMS leaders were eager to ensure the continued success of this new, yet important, industry.
In 1996, EMS stakeholders gathered to identify the most essential areas of EMS growth for the next twenty years. Their work resulted in the creation of a pivotal document called EMS Agenda for the Future. Ideas included in the Agenda helped steer some of the most important recent advancements of EMS — things like electronic patient records, evidence-based care, and information exchange. The document also highlighted the valuable role EMS providers could play in public health prevention efforts.
"In the future the success of EMS systems will be measured not only by the outcomes of their treatments, but also the results of their prevention efforts. Its expertise, resources, and positions in communities and the health care system make EMS an ideal candidate to serve lynchpin roles during multi-disciplinary, community-wide prevention initiatives. " -EMS Agenda for the Future, released 1996 Read the Full Text
This particular recommendation did not go unnoticed. Just four short years later, a joint meeting was convened by the National Highway Traffic Safety Administration (NHTSA) and the Health Resources and Services Administration (HRSA). EMS and Public Health officials from the National Association of EMS Physicians (NAEMSP) and the American Public Health Association (APHA) led the milestone effort. A snapshot of their discussions was distributed in the form of a bulletin after their first national meeting.
"On April 28, 2000 an unprecedented event took place which promises to have far reaching implications for healthcare. For the first time, representatives of national emergency medical services (EMS) and public health organizations came together to discuss strategies for joining forces...
Farsighted professionals from both disciplines began to envision how a collaboration between these complimentary services could result not only in improved efficiency for their traditional functions, but also in increased opportunities for reaching underserved segments of the community." EMS & Public Health Bulletin, released 2000 Read the Full Text
The bulletin's language conveys the participants' excitement and their strong feelings about future joint opportunities. However, subsequent meetings and further work were sidelined by the tragic events of September 11th, 2001. The effort was put on pause as our country (and the world) diverted its attention to more pressing matters.
Recently, the topic was reignited and brought back into the national spotlight. From 2016 to 2018, EMS leaders worked to update the EMS Agenda for the Future. The effort saw the creation of a new visionary document — EMS Agenda 2050. Proactive prevention programming by EMS was again a central theme.
"In a people-centered EMS system... EMS systems will be an integral piece of a public health and healthcare system focused on preventing injuries and illness, rather than simply responding to them." EMS Agenda 2050, released 2018 Read the Full Text
There is a clear consensus that EMS involvement in proactive, preventative programs are not only viable but incredibly valuable. The RAP Toolkit is designed to further advance this consensus into actionable guidance for California stakeholders through the creation of an easy, standardized approach to EMS and public health partnerships.
The Value of EMS in Public Health and Care Equity

EMS has a unique value in public health programming. It has the right providers, in the right place, and at the right time for impactful proactive prevention programming. EMTs and paramedics have an opportunity to deliver resources to individuals affected by a wide range of public health issues. Furthermore, the integration of public health programs into the EMS infrastructure has a special value in addressing community health inequities experienced by our rural and low-resource communities.
Individuals facing preventable health issues often seek care from their local 9-1-1 systems. Their use of the 9-1-1 system is often an indicator of increased needs relative to others within the affected population. This gives EMTs and paramedics unparalleled proximity to deliver critical resources to individuals with a demonstrated significant need.
Additionally, the public is (at least generally) familiar with the role of EMTs and paramedics as care providers who respond to these community health issues. Patients understand that the advice, opinions, or care delivered by these EMS professionals are anchored in this prior experience. This gives EMTs and paramedics improved leverage in potential prevention work.
Successful EMS public health initiatives harness both of these opportunities. They take advantage of the EMS providers' close proximity and timing with target populations. Additionally, they leverage the credibility and authenticity of EMS provider involvement to effect change.
It is important to note the value EMS providers bring to issues of care inequity facing California and our country. Not all counties and localities are equally resourced to proactively prevent injury and illness in their community. The infusion of public health programs into the already-existing EMS infrastructure can have immediate and large impacts for such rural or low-resource communities, and for relatively little investment. This makes EMS valuable efforts to ensure Californians do not face inequalities in health because of their race, socioeconomic status or location.
The Three Types of EMS Public Health Initiatives
The RAP Toolkit places EMS public health initiatives into three categories — educational, integrated, and expanded — based on how they utilize the existing EMS infrastructure.
Educational EMS Public Health Initiatives (PHIs)

Educational Public Health Initiatives (PHIs) provide EMTs and paramedics with information or training on specific preventable community health issues recognized in their local population. The information delivered by the Educational PHI promotes a better understanding of both the issue at hand and also the population it affects. This knowledge is carried by EMS providers throughout the community during normal EMS operations.
Examples of Educational PHIs:
1) A fire department provides its EMTs and Paramedics with cultural competence training for opioid use disorder and paths to recovery.
2) An EMS agency alerts its EMTs and Paramedics to an increase in senior falls, risk factors for falls, common strategies to prevent falls, and senior resources for families.
3) A fire department informs its EMTs and Paramedics of an increase in pediatric drownings and shares common causes, risk factors, and the best forms of prevention.
4) An EMS agency's ePCR data shows trends correlating to increased domestic violence. The agency educates its workforce on recognizing domestic violence, reporting policies, and resources for affected individuals.
Integrated EMS Public Health Initiatives (PHIs)

In contrast to Educational PHIs, which informally improve patient interactions and care through continuing education, Integrated PHIs bring formal prevention resources and surveillance into EMS 9-1-1 operations. Prevention resources are delivered to the affected populations during 9-1-1 interactions, and community health issues are surveilled through the real-time data offered by EMS patient care records and dispatch data. Integrated PHIs are often found to have the largest impact relative to the resources required for implementation because these lightweight programs are built right onto the existing 9-1-1 infrastructure in a non-disruptive manner.
Examples of Integrated PHIs:
1) An EMS agency uses ePCR and dispatch data for senior falls and shares this information regularly with public health stakeholders.
2) A fire department provides naloxone distribution to opioid overdose patients or bystanders during 9-1-1 incidents for use in future overdose events.
3) A fire department sets trigger alerts in its ePCR system for early identification of infectious disease outbreaks in coordination with their local department of public health.
4) An EMS agency transports substance abuse patients to specific receiving destinations that are prepared to address the individual's underlying needs and refer them to appropriate resources.
5) A fire department transports alcohol-intoxicated patients directly to a sobering center for appropriate care and addiction services.
Expanded EMS Public Health Initiatives (PHIs)

When communities recognize immense public health needs, it may be appropriate for EMS providers to do even more through the creation of Expanded PHIs. These initiatives build new services, programs, or efforts that are delivered in addition to normal EMS operations. Expanded PHIs may take the form of novel services delivered by specialty paramedics, such as community paramedics, in and around 9-1-1 incidents. They can also take the form of multidisciplinary taskforces, policy change workgroups, and other teams that operate entirely separate from normal 9-1-1 operations.
Examples of Expanded PHIs:
1) A fire department assigns a paramedic to an opioid task force that seeks out opioid users, provides buprenorphine as a bridging medication, and makes warm referrals to addiction services.
2) Local EMTs and paramedics meet with legislators or regional leadership regularly to positively impact policies addressing a community health issue.
3) An EMS agency deploys paramedics as a part of a regional vaccination task force to address endemic or other infectious diseases
4) A fire department utilizes community paramedics to help coordinate the care of 9-1-1 superusers who lack sufficient resources.
RAP Tool: The Problem Statement
Every RAP Tool shares the same anatomy designed to (1) qualify the community health issue, (2) quantify the community health issue, and (3) offer EMS public health initiatives to address the community health issue. The first step of qualifying the community health issue for EMS involvement is accomplished by the problem statement.
The problem statement describes the community health issue by answering a few key public health questions: What is occurring? What should be occurring? Who is affected and to what degree? What will happen if the problem is not addressed. These questions help shine a light on the causes, effects, and magnitude of the the issue at hand. Each RAP Tool Problem Statement then answers two EMS-specific questions: Do EMS providers have proximity to the issue? Do EMS providers have leverage with the public on the issue at hand?
You will recognize that these last two questions are directly extended from our discussion on the value of EMS in prevention programming. Together, these Problem Statement questions work together like a puzzle to qualify the impact of a community health issue and the need for EMS involvement in efforts to address it.
Example Problem Statement: The RAP Tool for Opioid Overdose and Death begins with an analysis of the opioid crisis in the United States. It identifies and validates a health gap currently present in many communities that see an increased incidence of opioid overdose and death. It maps out the direct causes of overdose and death due to opioid use disorder. It considers the indirect causes that may precipitate substance abuse. It identifies the primary and secondary injuries that will affect individuals and those around them if nothing is done. And finally, it validates that EMS is a frequent and regular care provider to this patient population and that EMS has meaningful programmatic opportunities to effect change.
RAP Tool: The Risk Assessment

The second component of every RAP Tool is a risk assessment, a quick and lightweight method to help you decide your own community's level of risk for the given community health issue. The level of community risk for a given health issue is important in weighing the appropriate level of resources and programming that should address that issue.
The risk assessment is built as three risk profiles — low, moderate, and high. Each profile contains data descriptors to which you can match your own community's data and rapidly identify a risk level. These data descriptors are carefully crafted through the consensus and work of stakeholder organizations and experts working in relevant areas of the healthcare continuum.
Example: The risk assessment for the Opioid Use RAP Tool provides three risk profiles from low to high that describe a regional risk level through overdose rates, naloxone use by EMS rates, and other ePCR trackable data. A locality with more than 15 opioid overdose deaths per 100,000 annually with correlated rates of overdose dispatches and naloxone administrations most closely matches the high-risk profile. Alternatively, a second region having less than 3 opioid overdose deaths per 100,000 annually, minimal overdose dispatches, and limited naloxone usage most closely matches the low-risk profile.
RAP Tool: Suggested Public Health Initiatives (PHIs)
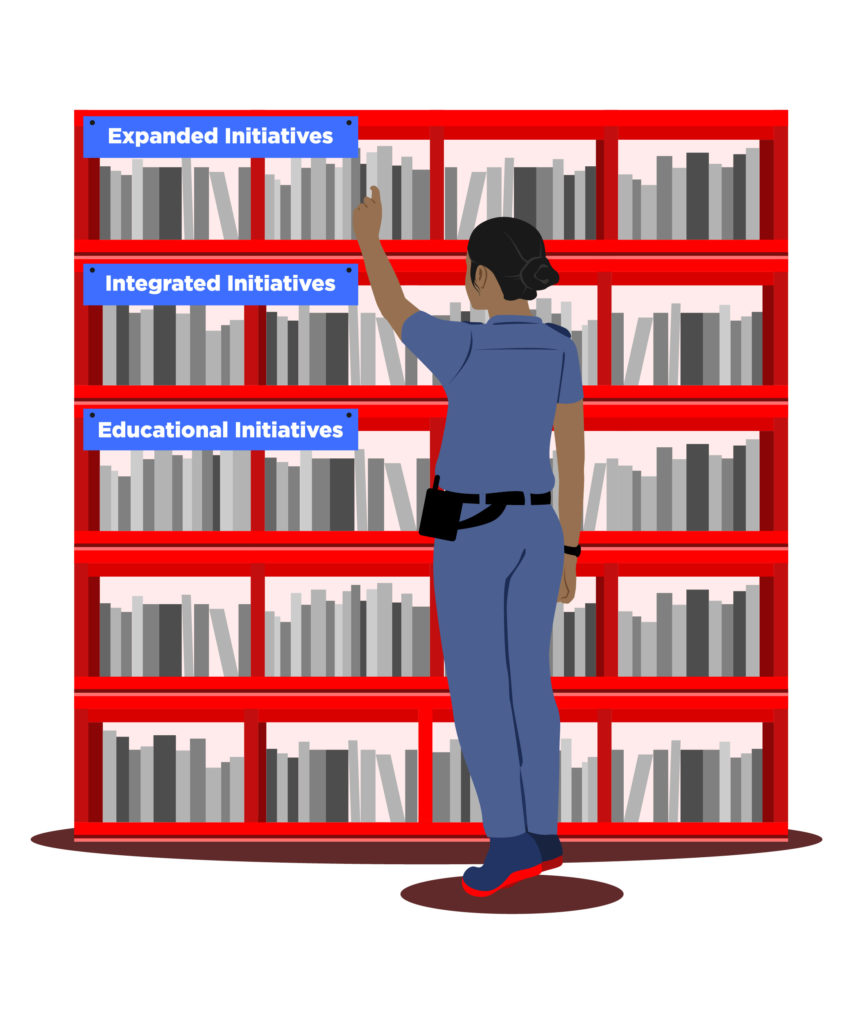
The third and final component of each RAP Tool is Suggested Public Health Initiatives (PHIs). These suggestions are made systematically by matching the progression of Risk Profiles (Low → Moderate → High) with the progression of PHI types we discussed earlier (Educational → Integrated → Expanded). This matching of risk level to initiative type ensures a correct allocation of resources for the identified level of community risk.
This progression of Suggested PHIs works as hierarchy in which high-complexity PHIs are supported by less-complex PHIs. This ensures that even the highest-level PHI implementations are still adequately tied to the broader workforce and leverage the core value EMS brings to public health programs.
Example: The Foundation's COPE Project uses the Opioid Use Disorder RAP Tool to recommend levels of EMS-led public health initiatives in communities across California. Areas of low risk (such as Fresno or San Bernardino Counties) are encouraged to provide Educational PHIs to their clinicians. Areas matching the moderate risk profile (such as Los Angeles County) are encouraged to implement Integrated PHIs such as naloxone distribution or referral information data collection in addition to supporting Educational PHIs. Areas with the highest risk (such as San Francisco City and County) are pointed towards Expanded PHIs such as opioid referral task forces and medication-assisted treatment and referral programs, in combination with supporting Educational and Integrated PHIs.
Bringing It All Together

We have seen how each RAP Tool shares a similar structure with three unique components. First, a RAP Tool qualifies the community health problem both generally and also for EMS involvement. Then, a RAP Tool gives the user a quick method for identifying their own community's risk for the given community health issue. Finally, a RAP tool translates this risk assessment into programmatic action. Each of these unique RAP Tool components answers a critical component in the program implementation and evaluation loop.
The problems, causes, and policy and program opportunities for a given public health issue are all readily identified within the issue's unique RAP Tool. Furthermore, the Risk Assessment creates a de facto quality assurance and improvement mechanism. By evaluating your position among the three risk profiles, you can continually assess the need for increased resources, decreased resources, or programmatic adjustments.
The utility of the RAP Toolkit in making EMS prevention program choices for standalone community health issues also supports the larger effort of creating a comprehensive EMS Prevention Plan, which considers and prioritizes EMS action across all of the public health issues facing a community. The use of the RAP Tools together as a cohesive entire Toolkit allows a community to efficiently calibrate their EMS prevention efforts to the needs of their community across diverse issues.
It is our hope that you find value in the RAP Toolkit, whether for a standalone EMS prevention program or an entire EMS prevention plan. Please do not hesitate to contact our team with any questions, needs, or suggestions!


